Exercise and cardiac health: physiological and molecular insights
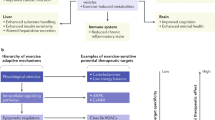
The cardiac benefits of exercise have been recognized for centuries. Studies have undisputedly shown that regular exercise is beneficial for the cardiovascular system in young, old, healthy and diseased populations. For these reasons, physical activity has been recommended worldwide for cardiovascular disease prevention and treatment. Although the benefits of exercise are clear, understanding of the molecular triggers that orchestrate these effects remains incomplete and has been a topic of intense research in recent years. Here, we provide a comprehensive review of the cardiac effects of physical activity, beginning with a brief history of exercise in cardiovascular medicine and then discussing seminal work on the physiological effects of exercise in healthy, diseased and aged hearts. Later, we revisit pioneering work on the molecular mechanisms underlying the cardiac benefits of exercise, and we conclude with our view on the translational potential of this knowledge as a powerful platform for cardiovascular disease drug discovery.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
133,45 € per year
only 11,12 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others

Exercise training maintains cardiovascular health: signaling pathways involved and potential therapeutics
Article Open access 01 September 2022
Exercise adaptations: molecular mechanisms and potential targets for therapeutic benefit
Article 06 July 2020

Molecular insights of exercise therapy in disease prevention and treatment
Article Open access 29 May 2024
References
- Ross, R. et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation134, e653–e699 (2016). ArticlePubMedGoogle Scholar
- Laukkanen, J. A. et al. Cardiovascular fitness as a predictor of mortality in men. Arch. Intern. Med.161, 825–831 (2001). ArticleCASPubMedGoogle Scholar
- Lavie, C. J. & Milani, R. V. Effects of cardiac rehabilitation, exercise training, and weight reduction on exercise capacity, coronary risk factors, behavioral characteristics, and quality of life in obese coronary patients. Am. J. Cardiol.79, 397–401 (1997). ArticleCASPubMedGoogle Scholar
- Marchionni, N. et al. Improved exercise tolerance and quality of life with cardiac rehabilitation of older patients after myocardial infarction: results of a randomized, controlled trial. Circulation107, 2201–2206 (2003). ArticlePubMedGoogle Scholar
- Roh, J., Rhee, J., Chaudhari, V. & Rosenzweig, A. The role of exercise in cardiac aging: from physiology to molecular mechanisms. Circ. Res.118, 279–295 (2016). ArticleCASPubMedPubMed CentralGoogle Scholar
- Wisløff, U., Helgerud, J., Kemi, O. J. & Ellingsen, O. Intensity-controlled treadmill running in rats: VO2 max and cardiac hypertrophy. Am. J. Physiol. Heart Circ. Physiol.280, H1301–H1310 (2001). ArticlePubMedGoogle Scholar
- Wisløff, U. et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation115, 3086–3094 (2007). ArticlePubMedGoogle Scholar
- Ramazzini, B. De morbis artificum diatriba [Diseases of workers]. 1713. Am. J. Public Health91, 1380–1382 (2001). ArticleCASPubMedPubMed CentralGoogle Scholar
- Hartley, P. H. & Llewellyn, G. F. Longevity of oarsmen. BMJ1, 657–662 (1939). ArticleCASPubMedPubMed CentralGoogle Scholar
- Morris, J. N., Heady, J. A., Raffle, P. A., Roberts, C. G. & Parks, J. W. Coronary heart-disease and physical activity of work. Lancet262, 1053–1057 (1953). ArticleCASPubMedGoogle Scholar
- Blair, S. N., Cheng, Y. & Holder, J. S. Is physical activity or physical fitness more important in defining health benefits? Med. Sci. Sports Exerc.33, S379–399 (2001). ArticleCASPubMedGoogle Scholar
- Dunn, A. L. et al. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. J. Am. Med. Assoc.281, 327–334 (1999). ArticleCASGoogle Scholar
- Blair, S. N. et al. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. J. Am. Med. Assoc.276, 205–210 (1996). ArticleCASGoogle Scholar
- Lee, D. C. et al. Leisure-time running reduces all-cause and cardiovascular mortality risk. J. Am. Coll. Cardiol.64, 472–481 (2014). ArticlePubMedPubMed CentralGoogle Scholar
- Ortega, F. B., Ruiz, J. R., Castillo, M. J. & Sjostrom, M. Physical fitness in childhood and adolescence: a powerful marker of health. Int. J. Obes.32, 1–11 (2008). ArticleCASGoogle Scholar
- Lee, I. M., Hsieh, C. C. & Paffenbarger, R. S. Jr. Exercise intensity and longevity in men: The Harvard Alumni Health Study. J. Am. Med. Assoc.273, 1179–1184 (1995). ArticleCASGoogle Scholar
- Wei, M. et al. Relationship between low cardiorespiratory fitness and mortality in normal-weight, overweight, and obese men. J. Am. Med. Assoc.282, 1547–1553 (1999). ArticleCASGoogle Scholar
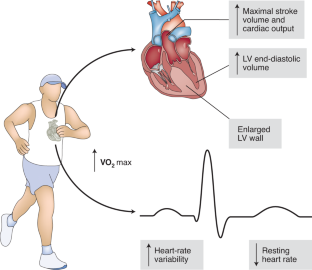
- Saltin, B. et al. Response to exercise after bed rest and after training. Circulation38, 1–78 (1968). The article describes changes in VO2max and cardiac variables as a result of 20 days of bed rest followed by 8 weeks of exercise training. ArticleGoogle Scholar
- Shephard, R. J. et al. The maximum oxygen intake: an international reference standard of cardiorespiratory fitness. Bull. World Health Organ.38, 757–764 (1968). CASPubMedPubMed CentralGoogle Scholar
- Wagner, P. D. Determinants of maximal oxygen transport and utilization. Annu. Rev. Physiol.58, 21–50 (1996). ArticleCASPubMedGoogle Scholar
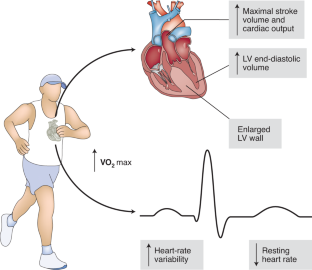
- Arbab-Zadeh, A. et al. Cardiac remodeling in response to 1 year of intensive endurance training. Circulation130, 2152–2161 (2014). ArticlePubMedPubMed CentralGoogle Scholar
- Zavorsky, G. S. Evidence and possible mechanisms of altered maximum heart rate with endurance training and tapering. Sports Med.29, 13–26 (2000). ArticleCASPubMedGoogle Scholar
- Pombo, J. F., Troy, B. L. & Russell, R. O. Jr. Left ventricular volumes and ejection fraction by echocardiography. Circulation43, 480–490 (1971). ArticleCASPubMedGoogle Scholar
- Morganroth, J., Maron, B. J., Henry, W. L. & Epstein, S. E. Comparative left ventricular dimensions in trained athletes. Ann. Intern. Med.82, 521–524 (1975). ArticleCASPubMedGoogle Scholar
- Fagard, R. H. Athlete’s heart: a meta-analysis of the echocardiographic experience. Int. J. Sports Med.17 (Suppl. 3), S140–S144 (1996). ArticlePubMedGoogle Scholar
- Spence, A. L. et al. A prospective randomised longitudinal MRI study of left ventricular adaptation to endurance and resistance exercise training in humans. J. Physiol. (Lond.)589, 5443–5452 (2011). ArticleCASGoogle Scholar
- McMullen, J. R. & Jennings, G. L. Differences between pathological and physiological cardiac hypertrophy: novel therapeutic strategies to treat heart failure. Clin. Exp. Pharmacol. Physiol.34, 255–262 (2007). ArticleCASPubMedGoogle Scholar
- Lovic, D. et al. Left ventricular hypertrophy in athletes and hypertensive patients. J. Clin. Hypertens. (Greenwich)19, 413–417 (2017). ArticleGoogle Scholar
- Iwasaki, K., Zhang, R., Zuckerman, J. H. & Levine, B. D. Dose-response relationship of the cardiovascular adaptation to endurance training in healthy adults: how much training for what benefit? J. Appl. Physiol.95, 1575–1583 (2003). ArticlePubMedGoogle Scholar
- Carter, J. B., Banister, E. W. & Blaber, A. P. Effect of endurance exercise on autonomic control of heart rate. Sports Med.33, 33–46 (2003). ArticlePubMedGoogle Scholar
- Sidhu, S. & Marine, J. E. Evaluating and managing bradycardia. Trends Cardiovasc. Med.30, 265–272 (2020). ArticlePubMedGoogle Scholar
- Saito, Y. et al. HCN4-overexpressing mouse embryonic stem cell-derived cardiomyocytes generate a new rapid rhythm in rats with bradycardia. Int. Heart J.59, 601–606 (2018). ArticleCASPubMedGoogle Scholar
- Nof, E., Antzelevitch, C. & Glikson, M. The contribution of HCN4 to normal sinus node function in humans and animal models. Pacing Clin. Electrophysiol.33, 100–106 (2010). ArticlePubMedGoogle Scholar
- Sneddon, J. F. & Camm, A. J. Sinus node disease: current concepts in diagnosis and therapy. Drugs44, 728–737 (1992). ArticleCASPubMedGoogle Scholar
- Levy, W. C. et al. Effect of endurance exercise training on heart rate variability at rest in healthy young and older men. Am. J. Cardiol.82, 1236–1241 (1998). ArticleCASPubMedGoogle Scholar
- Melanson, E. L. & Freedson, P. S. The effect of endurance training on resting heart rate variability in sedentary adult males. Eur. J. Appl. Physiol.85, 442–449 (2001). ArticleCASPubMedGoogle Scholar
- Carter, J. B., Banister, E. W. & Blaber, A. P. The effect of age and gender on heart rate variability after endurance training. Med. Sci. Sports Exerc.35, 1333–1340 (2003). ArticlePubMedGoogle Scholar
- Zingman, L. V. et al. Exercise-induced expression of cardiac ATP-sensitive potassium channels promotes action potential shortening and energy conservation. J. Mol. Cell. Cardiol.51, 72–81 (2011). ArticleCASPubMedPubMed CentralGoogle Scholar
- Fletcher, P. J., Pfeffer, J. M., Pfeffer, M. A. & Braunwald, E. Left ventricular diastolic pressure-volume relations in rats with healed myocardial infarction: effects on systolic function. Circ. Res.49, 618–626 (1981). ArticleCASPubMedGoogle Scholar
- Matsuda, Y. et al. Importance of left atrial function in patients with myocardial infarction. Circulation67, 566–571 (1983). ArticleCASPubMedGoogle Scholar
- Tanaka, M. et al. Quantitative analysis of myocardial fibrosis in normals, hypertensive hearts, and hypertrophic cardiomyopathy. Br. Heart J.55, 575–581 (1986). ArticleCASPubMedPubMed CentralGoogle Scholar
- Konhilas, J. P. et al. Exercise can prevent and reverse the severity of hypertrophic cardiomyopathy. Circ. Res.98, 540–548 (2006). ArticleCASPubMedGoogle Scholar
- De Angelis, K. et al. Exercise training changes autonomic cardiovascular balance in mice. J. Appl. Physiol.96, 2174–2178 (2004). ArticlePubMedGoogle Scholar
- Wisløff, U., Loennechen, J. P., Currie, S., Smith, G. L. & Ellingsen, Ø. Aerobic exercise reduces cardiomyocyte hypertrophy and increases contractility, Ca 2+ sensitivity and SERCA-2 in rat after myocardial infarction. Cardiovasc. Res.54, 162–174 (2002). ArticlePubMedGoogle Scholar
- Kemi, O. J. et al. Exercise training corrects control of spontaneous calcium waves in hearts from myocardial infarction heart failure rats. J. Cell. Physiol.227, 20–26 (2012). ArticleCASPubMedGoogle Scholar
- Qin, R. et al. Exercise training reduces ventricular arrhythmias through restoring calcium handling and sympathetic tone in myocardial infarction mice. Physiol. Rep.7, e13972 (2019). ArticlePubMedPubMed CentralCASGoogle Scholar
- Malmo, V. et al. Aerobic interval training reduces the burden of atrial fibrillation in the short term: a randomized trial. Circulation133, 466–473 (2016). ArticlePubMedGoogle Scholar
- Tjønna, A. E. et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: a pilot study. Circulation118, 346–354 (2008). ArticlePubMedPubMed CentralGoogle Scholar
- Hollekim-Strand, S. M. et al. High-intensity interval exercise effectively improves cardiac function in patients with type 2 diabetes mellitus and diastolic dysfunction: a randomized controlled trial. J. Am. Coll. Cardiol.64, 1758–1760 (2014). ArticlePubMedGoogle Scholar
- Kong, P., Christia, P. & Frangogiannis, N. G. The pathogenesis of cardiac fibrosis. Cell. Mol. Life Sci.71, 549–574 (2014). ArticleCASPubMedGoogle Scholar
- Weeks, K. L. et al. Phosphoinositide 3-kinase p110α is a master regulator of exercise-induced cardioprotection and PI3K gene therapy rescues cardiac dysfunction. Circ. Heart Fail5, 523–534 (2012). ArticleCASPubMedGoogle Scholar
- Ma, X. et al. Cardiac fibrosis alleviated by exercise training is AMPK-dependent. PLoS ONE10, e0129971 (2015). ArticlePubMedPubMed CentralCASGoogle Scholar
- Puhl, S. L. et al. Exercise attenuates inflammation and limits scar thinning after myocardial infarction in mice. Am. J. Physiol. Heart Circ. Physiol.309, H345–H359 (2015). ArticleCASPubMedGoogle Scholar
- Wilhelm, M. J. Long-term outcome following heart transplantation: current perspective. J. Thorac. Dis.7, 549–551 (2015). PubMedPubMed CentralGoogle Scholar
- Squires, R. W. Exercise training after cardiac transplantation. Med. Sci. Sports Exerc.23, 686–694 (1991). CASPubMedGoogle Scholar
- Tegtbur, U., Busse, M. W., Jung, K., Pethig, K. & Haverich, A. Time course of physical reconditioning during exercise rehabilitation late after heart transplantation. J. Heart Lung Transplant.24, 270–274 (2005). ArticlePubMedGoogle Scholar
- Karapolat, H. et al. Comparison of hospital-supervised exercise versus home-based exercise in patients after orthotopic heart transplantation: effects on functional capacity, quality of life, and psychological symptoms. Transplant. Proc.39, 1586–1588 (2007). ArticleCASPubMedGoogle Scholar
- Squires, R. W. et al. Partial normalization of the heart rate response to exercise after cardiac transplantation: frequency and relationship to exercise capacity. Mayo Clin. Proc.77, 1295–1300 (2002). ArticlePubMedGoogle Scholar
- Bowles, D. K. & Starnes, J. W. Exercise training improves metabolic response after ischemia in isolated working rat heart. J. Appl. Physiol.76, 1608–1614 (1994). ArticleCASPubMedGoogle Scholar
- French, J. P. et al. Exercise-induced protection against myocardial apoptosis and necrosis: MnSOD, calcium-handling proteins, and calpain. FASEB J.22, 2862–2871 (2008). ArticleCASPubMedPubMed CentralGoogle Scholar
- Powers, S. K. et al. Exercise training improves myocardial tolerance to in vivo ischemia-reperfusion in the rat. Am. J. Physiol.275, R1468–R1477 (1998). CASPubMedGoogle Scholar
- Yamashita, N. et al. Exercise provides direct biphasic cardioprotection via manganese superoxide dismutase activation. J. Exp. Med.189, 1699–1706 (1999). ArticleCASPubMedPubMed CentralGoogle Scholar
- Ejlersen, H. et al. Prognostic impact of physical activity prior to myocardial infarction: Case fatality and subsequent risk of heart failure and death. Eur. J. Prev. Cardiol.24, 1112–1119 (2017). ArticlePubMedGoogle Scholar
- Peytz, N. C. et al. Physical activity and risk of instant and 28-day case-fatality in myocardial infarction. PLoS ONE14, e0217398 (2019). ArticleCASPubMedPubMed CentralGoogle Scholar
- Brandfonbrener, M., Landowne, M. & Shock, N. W. Changes in cardiac output with age. Circulation12, 557–566 (1955). ArticleCASPubMedGoogle Scholar
- Lauer, M. S. et al. Impaired chronotropic response to exercise stress testing as a predictor of mortality. J. Am. Med. Assoc.281, 524–529 (1999). ArticleCASGoogle Scholar
- Leier, C. V., Heban, P. T., Huss, P., Bush, C. A. & Lewis, R. P. Comparative systemic and regional hemodynamic effects of dopamine and dobutamine in patients with cardiomyopathic heart failure. Circulation58, 466–475 (1978). ArticleCASPubMedGoogle Scholar
- Kappagoda, T. & Amsterdam, E. A. Exercise and heart failure in the elderly. Heart Fail. Rev.17, 635–662 (2012). ArticlePubMedGoogle Scholar
- Guarnieri, T., Filburn, C. R., Zitnik, G., Roth, G. S. & Lakatta, E. G. Contractile and biochemical correlates of beta-adrenergic stimulation of the aged heart. Am. J. Physiol.239, H501–H508 (1980). CASPubMedGoogle Scholar
- Zwiren, L. D., Freedson, P. S., Ward, A., Wilke, S. & Rippe, J. M. Estimation of VO2max: a comparative analysis of five exercise tests. Res. Q. Exerc. Sport62, 73–78 (1991). ArticleCASPubMedGoogle Scholar
- Lambert, M. I. & Noakes, T. D. Spontaneous running increases VO2max and running performance in rats. J. Appl. Phyisiol.68, 400–403 (1990). ArticleCASGoogle Scholar
- Leosco, D. et al. Exercise training and beta-blocker treatment ameliorate age-dependent impairment of beta-adrenergic receptor signaling and enhance cardiac responsiveness to adrenergic stimulation. Am. J. Physiol. Heart Circ. Physiol.293, H1596–H1603 (2007). ArticleCASPubMedGoogle Scholar
- Böhm, M. et al. Effects of exercise on myocardial adenylate cyclase and Gi alpha expression in senescence. Am. J. Physiol.264, H805–H814 (1993). PubMedGoogle Scholar
- Scarpace, P. J., Shu, Y. & Tumer, N. Influence of exercise training on myocardial beta-adrenergic signal transduction: differential regulation with age. J. Appl. Phyisiol.77, 737–741 (1994). ArticleCASGoogle Scholar
- Bers, D. M. Cardiac excitation-contraction coupling. Nature415, 198–205 (2002). ArticleCASPubMedGoogle Scholar
- Lim, C. C., Apstein, C. S., Colucci, W. S. & Liao, R. Impaired cell shortening and relengthening with increased pacing frequency are intrinsic to the senescent mouse cardiomyocyte. J. Mol. Cell. Cardiol.32, 2075–2082 (2000). ArticleCASPubMedGoogle Scholar
- Isenberg, G., Borschke, B. & Rueckschloss, U. Ca 2+ transients of cardiomyocytes from senescent mice peak late and decay slowly. Cell Calcium34, 271–280 (2003). ArticleCASPubMedGoogle Scholar
- Hamilton, S. & Terentyev, D. Altered intracellular calcium homeostasis and arrhythmogenesis in the aged heart. Int. J. Mol. Sci.20, E2386 (2019). ArticlePubMedCASGoogle Scholar
- Schmidt, U. et al. Restoration of diastolic function in senescent rat hearts through adenoviral gene transfer of sarcoplasmic reticulum Ca 2+ -ATPase. Circulation101, 790–796 (2000). ArticleCASPubMedGoogle Scholar
- Tate, C. A. et al. SERCA2a and mitochondrial cytochrome oxidase expression are increased in hearts of exercise-trained old rats. Am. J. Physiol.271, H68–H72 (1996). CASPubMedGoogle Scholar
- Iemitsu, M. et al. Exercise training improves cardiac function-related gene levels through thyroid hormone receptor signaling in aged rats. Am. J. Physiol. Heart Circ. Physiol.286, H1696–H1705 (2004). ArticleCASPubMedGoogle Scholar
- Biernacka, A. & Frangogiannis, N. G. Aging and cardiac fibrosis. Aging Dis.2, 158–173 (2011). PubMedPubMed CentralGoogle Scholar
- Olivetti, G., Melissari, M., Capasso, J. M. & Anversa, P. Cardiomyopathy of the aging human heart: myocyte loss and reactive cellular hypertrophy. Circ. Res.68, 1560–1568 (1991). ArticleCASPubMedGoogle Scholar
- Kwak, H. B. et al. Exercise training reduces fibrosis and matrix metalloproteinase dysregulation in the aging rat heart. FASEB J.25, 1106–1117 (2011). ArticleCASPubMedPubMed CentralGoogle Scholar
- Thomas, D. P., Cotter, T. A., Li, X., McCormick, R. J. & Gosselin, L. E. Exercise training attenuates aging-associated increases in collagen and collagen crosslinking of the left but not the right ventricle in the rat. Eur. J. Appl. Physiol.85, 164–169 (2001). ArticleCASPubMedGoogle Scholar
- Arbab-Zadeh, A. et al. Effect of aging and physical activity on left ventricular compliance. Circulation110, 1799–1805 (2004). ArticlePubMedGoogle Scholar
- Bernardo, B. C., Weeks, K. L., Pretorius, L. & McMullen, J. R. Molecular distinction between physiological and pathological cardiac hypertrophy: experimental findings and therapeutic strategies. Pharmacol. Ther.128, 191–227 (2010). ArticleCASPubMedGoogle Scholar
- Chesky, J. A., LaFollette, S., Travis, M. & Fortado, C. Effect of physical training on myocardial enzyme activities in aging rats. J. Appl. Physiol.55, 1349–1353 (1983). ArticleCASPubMedGoogle Scholar
- Short, K. R. et al. Decline in skeletal muscle mitochondrial function with aging in humans. Proc. Natl Acad. Sci. USA102, 5618–5623 (2005). ArticleCASPubMedPubMed CentralGoogle Scholar
- Ames, B. N., Shigenaga, M. K. & Hagen, T. M. Mitochondrial decay in aging. Biochim. Biophys. Acta1271, 165–170 (1995). ArticlePubMedGoogle Scholar
- Escobales, N. et al. Mitochondria-targeted ROS scavenger improves post-ischemic recovery of cardiac function and attenuates mitochondrial abnormalities in aged rats. J. Mol. Cell. Cardiol.77, 136–146 (2014). ArticleCASPubMedPubMed CentralGoogle Scholar
- Hosseini, L., Vafaee, M. S. & Badalzadeh, R. Melatonin and nicotinamide mononucleotide attenuate myocardial ischemia/reperfusion injury via modulation of mitochondrial function and hemodynamic parameters in aged rats. J. Cardiovasc. Pharmacol. Ther.25, 240–250 (2020). ArticleCASPubMedGoogle Scholar
- Boengler, K., Kosiol, M., Mayr, M., Schulz, R. & Rohrbach, S. Mitochondria and ageing: role in heart, skeletal muscle and adipose tissue. J. Cachexia Sarcopenia Muscle8, 349–369 (2017). ArticlePubMedPubMed CentralGoogle Scholar
- Judge, S. et al. Exercise by lifelong voluntary wheel running reduces subsarcolemmal and interfibrillar mitochondrial hydrogen peroxide production in the heart. Am. J. Physiol. Regul. Integr. Comp. Physiol.289, R1564–R1572 (2005). ArticleCASPubMedGoogle Scholar
- Picard, M. et al. Acute exercise remodels mitochondrial membrane interactions in mouse skeletal muscle. J. Appl. Phyisiol.115, 1562–1571 (2013). ArticleCASGoogle Scholar
- Wang, H. et al. Exercise prevents cardiac injury and improves mitochondrial biogenesis in advanced diabetic cardiomyopathy with PGC-1α and Akt activation. Cell Physiol. Biochem.35, 2159–2168 (2015). ArticleCASPubMedGoogle Scholar
- Bergmann, O. et al. Evidence for cardiomyocyte renewal in humans. Science324, 98–102 (2009). ArticleCASPubMedPubMed CentralGoogle Scholar
- Laugwitz, K. L. et al. Postnatal isl1 + cardioblasts enter fully differentiated cardiomyocyte lineages. Nature433, 647–653 (2005). ArticleCASPubMedPubMed CentralGoogle Scholar
- Lázár, E., Sadek, H. A. & Bergmann, O. Cardiomyocyte renewal in the human heart: insights from the fall-out. Eur. Heart J.38, 2333–2342 (2017). ArticlePubMedPubMed CentralCASGoogle Scholar
- Vujic, A. et al. Exercise induces new cardiomyocyte generation in the adult mammalian heart. Nat. Commun.9, 1659 (2018). ArticlePubMedPubMed CentralCASGoogle Scholar
- Mazzeo, R. S. & Tanaka, H. Exercise prescription for the elderly: current recommendations. Sports Med.31, 809–818 (2001). ArticleCASPubMedGoogle Scholar
- Singh, M. A. Exercise comes of age: rationale and recommendations for a geriatric exercise prescription. J. Gerontol. A Biol. Sci. Med. Sci.57, M262–M282 (2002). ArticlePubMedGoogle Scholar
- Gomes Neto, M. et al. High intensity interval training versus moderate intensity continuous training on exercise capacity and quality of life in patients with heart failure with reduced ejection fraction: a systematic review and meta-analysis. Int. J. Cardiol.261, 134–141 (2018). ArticlePubMedGoogle Scholar
- Rognmo, Ø. et al. Cardiovascular risk of high- versus moderate-intensity aerobic exercise in coronary heart disease patients. Circulation126, 1436–1440 (2012). ArticlePubMedGoogle Scholar
- Chien, K. R., Knowlton, K. U., Zhu, H. & Chien, S. Regulation of cardiac gene expression during myocardial growth and hypertrophy: molecular studies of an adaptive physiologic response. FASEB J.5, 3037–3046 (1991). ArticleCASPubMedGoogle Scholar
- Strøm, C. C. et al. Expression profiling reveals differences in metabolic gene expression between exercise-induced cardiac effects and maladaptive cardiac hypertrophy. FEBS J.272, 2684–2695 (2005). ArticlePubMedCASGoogle Scholar
- Song, H. K., Hong, S. E., Kim, T. & Kim, D. H. Deep RNA sequencing reveals novel cardiac transcriptomic signatures for physiological and pathological hypertrophy. PLoS ONE7, e35552 (2012). ArticleCASPubMedPubMed CentralGoogle Scholar
- Bernardo, B. C., Ooi, J. Y. Y., Weeks, K. L., Patterson, N. L. & McMullen, J. R. Understanding key mechanisms of exercise-induced cardiac protection to mitigate disease: current knowledge and emerging concepts. Physiol. Rev.98, 419–475 (2018). ArticleCASPubMedGoogle Scholar
- Alessio, H. M., Ansinelli, H., Threadgill, C. & Hagerman, A. E. Comparison of gene and protein expressions in rats residing in standard cages with those having access to an exercise wheel. BioMed. Res. Int.2014, 950516 (2014). ArticlePubMedPubMed CentralCASGoogle Scholar
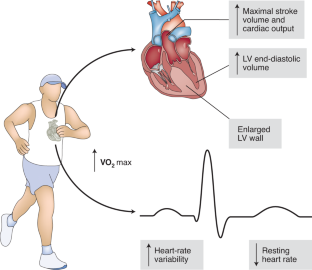
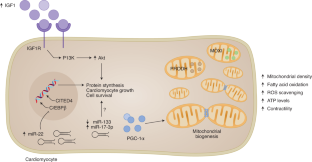
- Puigserver, P. et al. A cold-inducible coactivator of nuclear receptors linked to adaptive thermogenesis. Cell92, 829–839 (1998). ArticleCASPubMedGoogle Scholar
- Baar, K. et al. Adaptations of skeletal muscle to exercise: rapid increase in the transcriptional coactivator PGC-1. FASEB J.16, 1879–1886 (2002). ArticleCASPubMedGoogle Scholar
- Botta, A. et al. Short term exercise induces PGC-1α, ameliorates inflammation and increases mitochondrial membrane proteins but fails to increase respiratory enzymes in aging diabetic hearts. PLoS ONE8, e70248 (2013). ArticleCASPubMedPubMed CentralGoogle Scholar
- Arany, Z. et al. Transcriptional coactivator PGC-1α controls the energy state and contractile function of cardiac muscle. Cell Metab.1, 259–271 (2005). The article shows how PGC-1α functions as a major regulator of bioenergetics in cardiac muscle. ArticleCASPubMedGoogle Scholar
- Scarpulla, R. C., Vega, R. B. & Kelly, D. P. Transcriptional integration of mitochondrial biogenesis. Trends Endocrinol. Metab.23, 459–466 (2012). ArticleCASPubMedPubMed CentralGoogle Scholar
- Dufour, C. R. et al. Genome-wide orchestration of cardiac functions by the orphan nuclear receptors ERRalpha and gamma. Cell Metab.5, 345–356 (2007). ArticleCASPubMedGoogle Scholar
- Moreira, J. B. N. et al. Exercise reveals proline dehydrogenase as a potential target in heart failure. Prog. Cardiovasc. Dis.62, 193–202 (2019). ArticlePubMedGoogle Scholar
- Makarewich, C. A. et al. MOXI Is a mitochondrial micropeptide that enhances fatty acid β-oxidation. Cell Rep.23, 3701–3709 (2018). ArticleCASPubMedPubMed CentralGoogle Scholar
- McMullen, J. R. et al. Phosphoinositide 3-kinase(p110α) plays a critical role for the induction of physiological, but not pathological, cardiac hypertrophy. Proc. Natl Acad. Sci. USA100, 12355–12360 (2003). This article shows that PI3K is required for the induction of physiological cardiac growth and is essential for maintaining contractile function in response to pathological stimuli. ArticleCASPubMedPubMed CentralGoogle Scholar
- McMullen, J. R. et al. Protective effects of exercise and phosphoinositide 3-kinase(p110α) signaling in dilated and hypertrophic cardiomyopathy. Proc. Natl Acad. Sci. USA104, 612–617 (2007). ArticleCASPubMedPubMed CentralGoogle Scholar
- DeBosch, B. et al. Akt1 is required for physiological cardiac growth. Circulation113, 2097–2104 (2006). ArticleCASPubMedGoogle Scholar
- Kim, J. et al. Insulin-like growth factor I receptor signaling is required for exercise-induced cardiac hypertrophy. Mol. Endocrinol.22, 2531–2543 (2008). ArticleCASPubMedPubMed CentralGoogle Scholar
- McMullen, J. R. et al. The insulin-like growth factor 1 receptor induces physiological heart growth via the phosphoinositide 3-kinase(p110α) pathway. J. Biol. Chem.279, 4782–4793 (2004). ArticleCASPubMedGoogle Scholar
- Boudina, S. et al. Contribution of impaired myocardial insulin signaling to mitochondrial dysfunction and oxidative stress in the heart. Circulation119, 1272–1283 (2009). ArticleCASPubMedPubMed CentralGoogle Scholar
- Noh, J. et al. Phosphoinositide dependent protein kinase 1 is required for exercise-induced cardiac hypertrophy but not the associated mitochondrial adaptations. J. Mol. Cell. Cardiol.89, 297–305 (2015). ArticleCASPubMedPubMed CentralGoogle Scholar
- Kim, A. H., Khursigara, G., Sun, X., Franke, T. F. & Chao, M. V. Akt phosphorylates and negatively regulates apoptosis signal-regulating kinase 1. Mol. Cell. Biol.21, 893–901 (2001). ArticleCASPubMedPubMed CentralGoogle Scholar
- Weeks, K. L., Bernardo, B. C., Ooi, J. Y. Y., Patterson, N. L. & McMullen, J. R. The IGF1-PI3K-Akt signaling pathway in mediating exercise-induced cardiac hypertrophy and protection. Adv. Exp. Med. Biol.1000, 187–210 (2017). ArticleCASPubMedGoogle Scholar
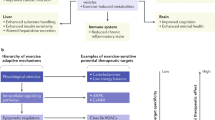
- Vega, R. B., Konhilas, J. P., Kelly, D. P. & Leinwand, L. A. Molecular mechanisms underlying cardiac adaptation to exercise. Cell Metab.25, 1012–1026 (2017). ArticleCASPubMedPubMed CentralGoogle Scholar
- Silva, G. J. J., Bye, A., El Azzouzi, H. & Wisløff, U. MicroRNAs as important regulators of exercise adaptation. Prog. Cardiovasc. Dis.60, 130–151 (2017). ArticlePubMedGoogle Scholar
- Shi, J. et al. miR-17-3p contributes to exercise-induced cardiac growth and protects against myocardial ischemia-reperfusion injury. Theranostics7, 664–676 (2017). ArticleCASPubMedPubMed CentralGoogle Scholar
- Carè, A. et al. MicroRNA-133 controls cardiac hypertrophy. Nat. Med.13, 613–618 (2007). ArticlePubMedCASGoogle Scholar
- Liu, X. et al. miR-222 is necessary for exercise-induced cardiac growth and protects against pathological cardiac remodeling. Cell Metab.21, 584–595 (2015). ArticleCASPubMedPubMed CentralGoogle Scholar
- Boström, P. et al. C/EBPβ controls exercise-induced cardiac growth and protects against pathological cardiac remodeling. Cell143, 1072–1083 (2010). ArticlePubMedPubMed CentralCASGoogle Scholar
- Bezzerides, V. J. et al. CITED4 induces physiologic hypertrophy and promotes functional recovery after ischemic injury. JCI Insight1, e85904 (2016). ArticlePubMedPubMed CentralGoogle Scholar
- Hamilton, K. L. et al. Exercise, antioxidants, and HSP72: protection against myocardial ischemia/reperfusion. Free Radic. Biol. Med.34, 800–809 (2003). ArticleCASPubMedGoogle Scholar
- Hutter, J. J. et al. Overexpression of heat shock protein 72 in transgenic mice decreases infarct size in vivo. Circulation94, 1408–1411 (1996). ArticleCASPubMedGoogle Scholar
- Tekin, D., Dursun, A. D. & Xi, L. Hypoxia inducible factor 1 (HIF-1) and cardioprotection. Acta Pharmacol. Sin.31, 1085–1094 (2010). ArticleCASPubMedPubMed CentralGoogle Scholar
- Brown, D. A. et al. Cardioprotection afforded by chronic exercise is mediated by the sarcolemmal, and not the mitochondrial, isoform of the KATP channel in the rat. J. Physiol. (Lond.)569, 913–924 (2005). ArticleCASGoogle Scholar
- Yao, Z. & Gross, G. J. Effects of the KATP channel opener bimakalim on coronary blood flow, monophasic action potential duration, and infarct size in dogs. Circulation89, 1769–1775 (1994). ArticleCASPubMedGoogle Scholar
- Wang, Z. et al. Irisin protects heart against ischemia-reperfusion injury through a SOD2-dependent mitochondria mechanism. J. Cardiovasc. Pharmacol.72, 259–269 (2018). ArticleCASPubMedPubMed CentralGoogle Scholar
- Otaka, N. et al. Myonectin is an exercise-induced myokine that protects the heart from ischemia-reperfusion injury. Circ. Res.123, 1326–1338 (2018). ArticleCASPubMedGoogle Scholar
- Tham, Y. K. et al. Lipidomic profiles of the heart and circulation in response to exercise versus cardiac pathology: a resource of potential biomarkers and drug targets. Cell Rep.24, 2757–2772 (2018). ArticleCASPubMedGoogle Scholar
- Guo, H., Isserlin, R., Emili, A. & Burniston, J. G. Exercise-responsive phosphoproteins in the heart. J. Mol. Cell. Cardiol.111, 61–68 (2017). ArticleCASPubMedGoogle Scholar
- Penny, W. F. & Hammond, H. K. Randomized clinical trials of gene transfer for heart failure with reduced ejection fraction. Hum. Gene Ther.28, 378–384 (2017). ArticleCASPubMedPubMed CentralGoogle Scholar
- Narkar, V. A. et al. AMPK and PPARdelta agonists are exercise mimetics. Cell134, 405–415 (2008). ArticleCASPubMedPubMed CentralGoogle Scholar
Acknowledgements
J.B.N.M. is supported by a grant from the Research Council of Norway (project 275714). M.W. is supported by grants from the KG Jebsen Center for Exercise in Medicine and the Liaison Committee between the Central Norway Regional Health Authority (RHA) and the Norwegian University of Science and Technology (NTNU).